by Moshood Isah
Hypertension is a major public health problem in Nigeria, with prevalence of 37.5%. This means that nearly 4 out of 10 Nigerian adults have hypertension. Similarly the prevalence of diabetes is increasing worldwide, and Nigeria is no exception; an estimated 7% of adults in Nigeria have diabetes, making it among the most common cardiovascular diseases in the country.
Unfortunately, lack of access to quality and affordable hypertension and diabetes services in rural communities and primary health care is a major concern. This is largely due to disparity in access to quality healthcare, especially between rural and urban areas in Nigeria as a result of economic, social, geographic, and health workforce factors. For instance, the secondary health facilities where the few drugs are, with the facility for testing and the medical professionals are far from the rural communities, making access difficult. This is exacerbated by the high cost of medications, making it difficult for some clients to afford the treatment they need, resulting in low treatment outcomes.
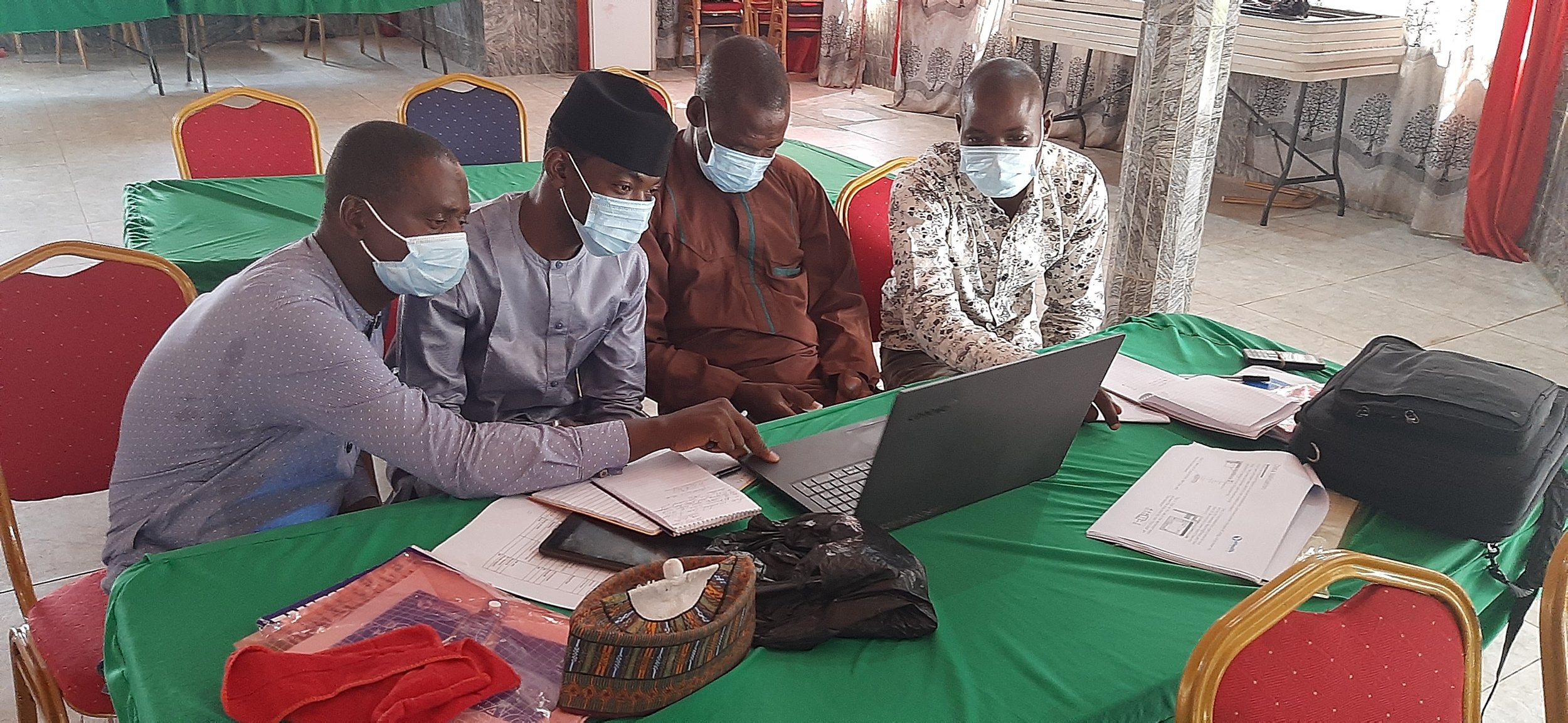
Thus, adapting and digitizing the World Health Organisation Package of Essential Noncommunicable (PEN) disease interventions for primary health care, eHealth Africa is collaborating with the EHA Clinic Reaching Everyone with Accessible Community Healthcare (REACH) program to reach out to marginalized communities with healthcare interventions. This, according to the Project Manager Lucy Okoye, is aimed at improving access to quality care and affordable services for persons with hypertension and diabetes and others at risk.
She said, “Social mobilization activities will increase rural communities' knowledge of hypertension and diabetes”, saying the identification of risk factors and the signs of hypertension and diabetes will likely result in the adoption of a preventive healthy lifestyle and prompt seeking of treatment. Another potential impact of the intervention according to her is to reduce the prevalence of hypertension and diabetes and improve the health and well-being of the target communities, helping people to live longer and lead healthier lives.
In February, eHealth Africa supported the free medical outreach conducted in the Kuje community of the Federal Capital Territory and Gyadi-Gyadi community of Kano state. According to Adawiya, Mahmud Ila, Product and Quality Assurance Coordinator at the EHA REACH clinic said the outreach is an opportunity to reach the people accessible and to provide free healthcare within the community.
“We are having an outreach where we see hypertension and diabetic patients,we measure the blood pressure and fasten blood sugar.” If there is a need for us to give hypertensive and glycine medication we give them which is going to be free for 6 months”, she said.
She said, the economic realities in developing countries like Nigeria limits citizens especially the older generation from accessing good medical care. She said, “You know how the economy is in Nigeria; economically it's hard for them to go to the hospital so we are just trying to make an impact in the community”.
Speaking on community acceptance and mobilization strategy for the outreach, Adawiya said, the partners leveraged on its Community Health Extension Workers (CHEW) to discuss the impact of the intervention with traditional leaders and community influencers.
Community Feedback
Zainab Abdullahi is a resident of Kasuwan Dare area of Gyadi-Gyadi community of Kano state. She heard of the REACH Clinic Outreach through community influencers. “Now they checked our BP,Blood sugar level and from here we will proceed to see the doctor”, she said.
Zainab lauded the outreach initiative saying the community is receptive to ideas like this. “the hospital environment is clean and welcoming and this is why you can see close to 100 people coming for this outreach”. “If they can spread their tentacles and establish this kind of hospital in all areas, we will be happy so that everyone will visit the nearest hospital rather than going far from home to access healthcare”, she said. There is also a need to have additional doctors to attend to a growing number of patients in a bid to reduce waiting time, she said.
Ahmed Salisu Musa has spent 45 years in the community. He expressed his excitement saying the outreach has brought good healthcare delivery to his doorstep. “They took my blood samples, gave me some medications and I was told, I am not diabetic”, he said
He said, “as a community leader myself, I am glad to have witnessed what is happening and will pull in more people to come and get checked.” Musa called for increased mobilization of citizens and more importantly expansion of the intervention to reach other communities.